It’s a fact that women utilize healthcare services more than men, with estimates at approximately 33% more often. In the US women’s pursuit of gynecological exams, annual check-ups, and preventive care totals roughly $15 billion dollars more than that spent by men. On the other hand men tend to seek care less but utilize hospitalization more, perhaps due to the progression of unaddressed problems. These differences in approach may stem from multiple factors: personality, culture, tolerance, resources, and lack of research on some issues. The complexity of the female reproductive system can explain some of this disparity but not all, as many of these statistics exclude childbirth.
When discussing women’s health, some confine the topic to the pelvic region and pelvic floor. I want to think broader and briefly explore multiple issues:
- Anxiety / depression
- Autoimmune
- Digestive
- Eating
- Gynecological including menstrual, childbirth, breast health, & menopause
- Headaches
- Heart disease
- Hypermobility
- Myofascial pain
- Osteoporosis
- Urinary
- Weight
Many of these problems often co-exist: heart and bladder issues (stemming from their relationship in the fascia), hypermobility and myofascial pain, and digestive and anxiety issues, for example. While statistics vary greatly for occurrence in men versus women, for the most part women struggle with most of these at higher rates (of course gynecological issues). A surprising exception is weight: more men are overweight than women, but more women are significantly overweight / obese than men. Heart disease is the leading cause of death for more men than women in the US, but more women are afflicted later in life. Globally women tend to live longer than men, perhaps in part due to the tendency to address health issues sooner. While longevity is admirable, high quality of life is intuitively more desirable yet often frustratingly elusive for many.
"One potentially influential factor on these disparities may stem from hormonal differences between men and women, as well receptors in the fascia."
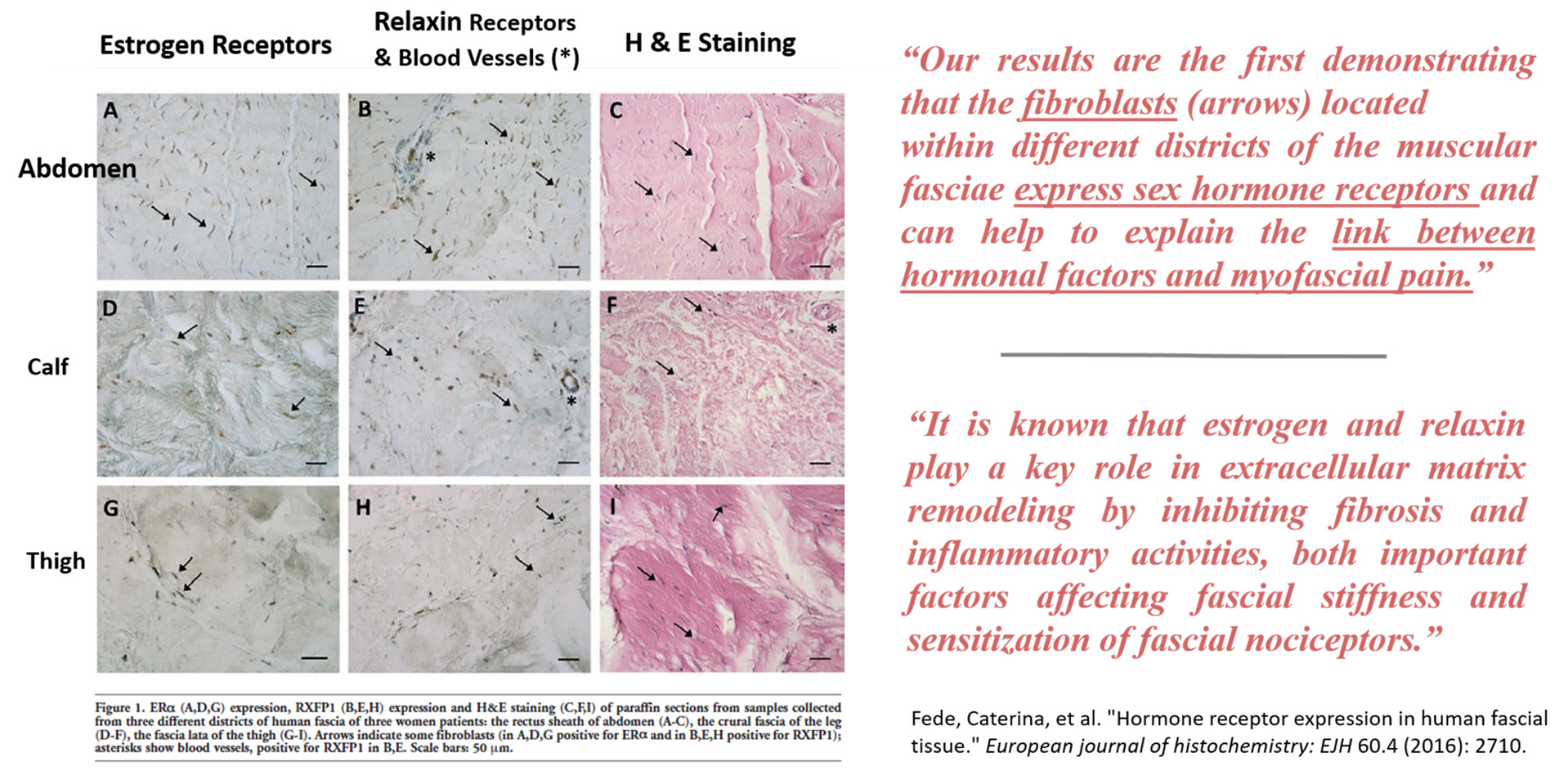
One potentially influential factor on these disparities may stem from hormonal differences between men and women, as well receptors in the fascia. Research shows that fibroblasts (cells producing collagen, elastin, and much more) in the muscular fascia possess receptors for estrogen and relaxin which are key sex hormones for women and less so for men. These hormones play a vital role in the remodeling of the tissues and thereby preventing stiffness, pain, and inflammation. Fluctuations in the levels of these hormones can severely impact the status of the connective tissues and their ability to promote normal function of the musculoskeletal and internal organ systems. While men produce these hormones, they are at much lower levels and not subject to the extreme fluctuations that regularly occur throughout a woman’s life with the menstrual cycle, childbirth, and menopause.
Certainly multiple factors can impact a woman’s health (as anyone’s) and the below diagram depicts this construct. The International Association for the Study of Pain (IASP) published this chart in 2009 to reflect the multi-faceted nature of pain. The word “pain” could be replaced with many words: symptoms, disease, stiffness, disability, or dysfunction. The point remains that most problems do not have one isolated source, but rather a combination of influential factors which are differently weighted for different individuals. A death or divorce could put more emphasis on the emotional state for one person. In the case of many women, the daily demands of balancing work, home, children, grandchildren, and aging parents can overload several factors. One may successfully deal with many of these influences all the time. But when the weight of one segment is increased, or a new element is added, then it may be enough to tip the scale into overload and dysfunction. This is especially true for those who constantly dwell precariously on the edge of wellness versus dysfunction - a good reason to move yourself from the edge.
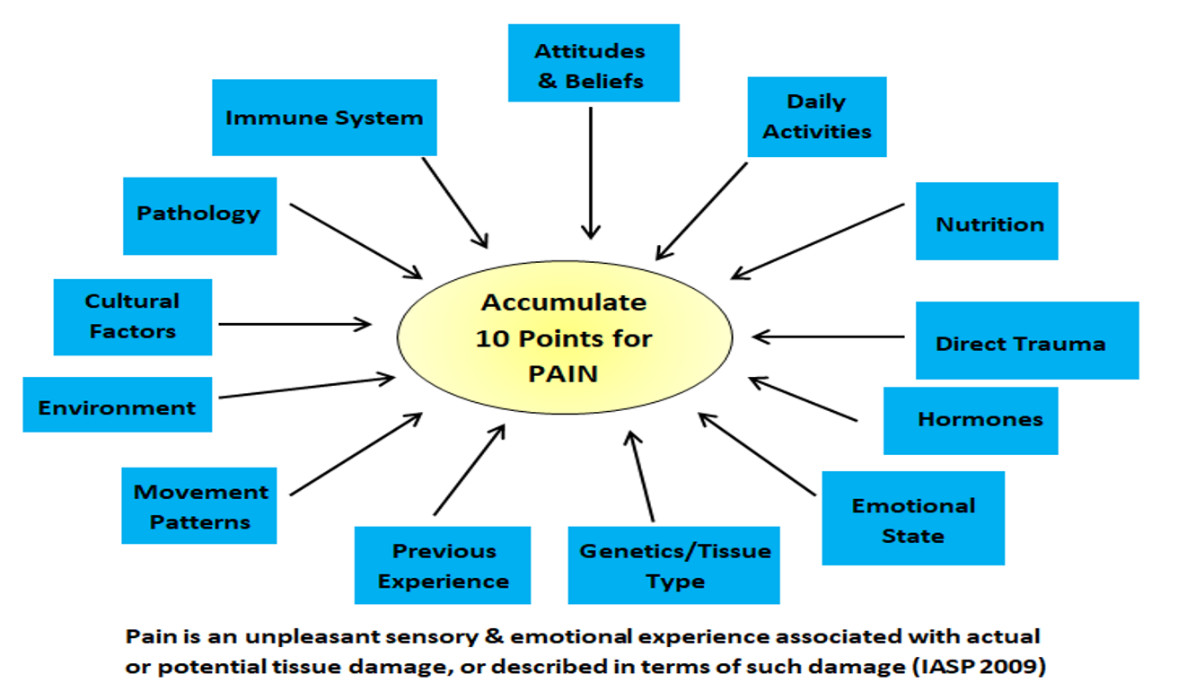
- We are not robots, we are humans with multiple limitations. We can’t do it all and continue to function happily and healthily. Rest and recreation are essential to our well-being.
- Fascia is influenced by daily activities, nutrition, direct trauma, hormones, emotions, genetics, movement patterns, environment, pathology, and the immune system. Good input from these elements can equate with good fascial function for the musculoskeletal and internal organ systems. Bad input from these elements can cause fascial dysfunction.
- Conversely, fascial dysfunction can negatively influence the performance of daily activities, hormones, emotions, movement patterns, pathology, and the immune system. This can lead to pain, altered movement, and disease.
- Change what you can, and what you can’t change maybe won’t be so impactful. You can’t change your genetics, previous experiences, or trauma. But if you change elements you can control, like daily activities, movement patterns, nutrition, and attitudes & beliefs then maybe those factors out of control will be less impactful, move you from the edge of dysfunction, and result in a better state of wellness.
- Quick Tips: Break up periods of sitting to give the pelvic segment and hips a change; Stretching and moving are good, but don't overstretch (palming floor, face to knees, splits, hyperextending knees and elbows); Minimize bladder irritants (caffeine, alcohol, acidic foods, and certain spices).
If you are a woman struggling with your body consider that there are options beyond what mainstream health care and the media promote. Very often what seems to be disease and dysfunction of an organ (bladder, ovaries, uterus, stomach, heart, breast, etc.) can be dysfunction of the fascial environment surrounding the organ. One novel study found that stretching the connective tissues helped prevent cancer in mice, and they proposed applications to breast cancer research. Knowledge of and attention to the fascia in research and clinical practice has been neglected in mainstream health care, but is gaining traction. Please consider these constructs before you resort to multiple tests, prescription medications, and surgery. To learn more about how fascial work may help a multitude of women’s issues please give me a call, send a text, book an exploratory session, or schedule a consult. You have options – act on them!
- Bertakis, Klea D., et al. "Gender differences in the utilization of health care services." Journal of family practice 49.2 (2000).
- Yan, Brandon W., et al. "Widening gender gap in life expectancy in the US, 2010-2021." JAMA Internal Medicine 184.1 (2024): 108-110.
- Pasini, Andrea, Sfriso, Maria, and Stecco, Carla. "Treatment of chronic pelvic pain with Fascial Manipulation®." Pelviperineology 35.1 (2016): 13.
- Fede, Caterina, et al. "Hormone receptor expression in human fascial tissue." European journal of histochemistry: EJH 60.4 (2016): 2710.
- Critchley, Hilary OD, et al. "Menstruation: science and society." American journal of obstetrics and gynecology 223.5 (2020): 624-664.
- He, Yi, et al. "A novel mouse model of voluntary stretching and its application in breast cancer research." bioRxiv (2025): 2025-01.





